What is the difference between overweight and obese
Overweight vs. Obese
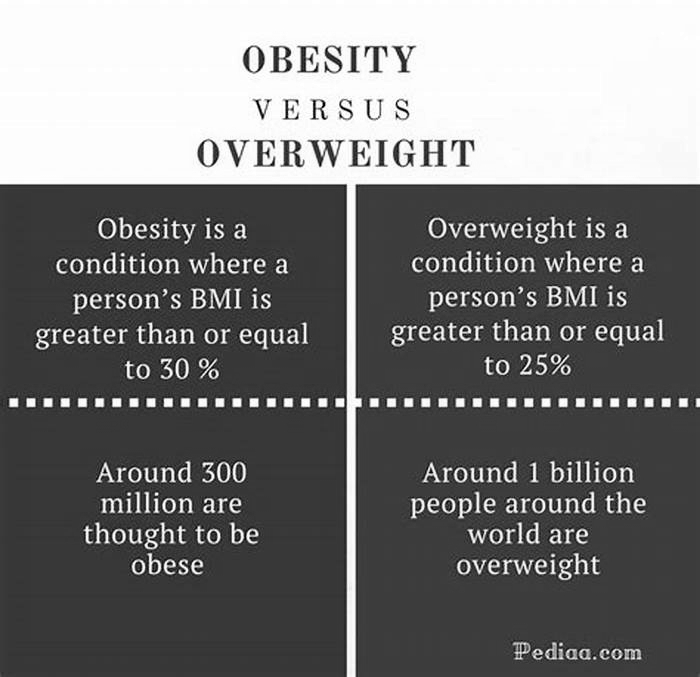
Both Overweight and Obesity imply a condition of excess weight of a person.
Being overweight means having more body weight than is considered normal or healthy for ones age or build. On the other hand, obesity is the condition of being obese, i.e., excess amount of body fat with a BMI of over 30. While an overweight person will carry excess weight, he may or may not have excess accumulation of fat.
What is Obesity?
The medical definition of obesity in an adult is as follows:
Obesity is a condition where an individual accumulates excessive fat in the body, indicated by a body mass index of 30 or greater.
Obesity is excess fat compared to lean body mass, or a body weight that is 30 percent over the ideal weight for a specific height. A person is obese when the amount of adipose tissue is sufficiently high. Obesity is a chronic disorder, caused by complex variety of factors.
What is BMI?
The range that is considered "normal" or healthy weight depends upon a person's height. It is natural for taller people to weigh more. BMI stands for Body Mass Index. It is a number that is calculated based on both the height and weight to determine if the weight is high or low compared with what you would expect for that height. BMI indicator of body fatness, and is used as a screening tool for weight issues.
How to Calculate BMI
BMI = W / (H2) where W is the person's weight (in kilograms, not pounds) and H is the person's height (in meters). In other words, BMI is a person's weight (in kilograms) divided by the square of height (in meters).
If weight is in pounds and height is in inches, then BMI is calculated using a similar formula, only multiplying by 703. i.e., 703 * W / (H2), where W is the weight in lbs and H is the height in inches.
An easier way to find out your BMI is to use a BMI calculator or look up this reference table or the chart below.
Calculating Normal or Healthy Weight
What does BMI indicate?
Adults are grouped into the following categories based on BMI (body mass index):
- BMI less than 18.5: Underweight
- BMI 18.5 to 24.9: Healthy weight range
- BMI 25.0 to 29.9: Overweight
- BMI more than 30: Obese
- BMI 3035: Moderately obese (Obese Class I)
- BMI 3540: Severely obese (Obese Class II)
- BMI > 40: Morbidly obese (Obese Class III)

This BMI chart shows BMI ranges for different height and weight combinations. Height can be in meters or feet and inches; weight can be looked up both in kilograms and pounds.
It should be noted, however, that BMI calculations can be misleading.[1] Those considered overweight or obese may in comes cases be healthier than someone who appears to be conventionally healthy.
What causes excess weight?
Overweight is weighing more than the typical weight range given your age, sex, and height. Being overweight does not necessarily imply excess fat. People like athletes and bodybuilders can be overweight but not obese.
Overeating is not the only reason someone might be overweight; other causes include a sedentary lifestyle with no exercise, metabolic or eating disorders, or medical conditions like thyroid problems or other types of hormonal imbalance. Disabilities that inhibit exercise, and food allergies can also contribute to someone being overweight or even obese.
Psychological conditions can further contribute to weight issues and make treating them difficult. For example, it is possible for someone who is bulimic to be overweight at the same time.
Risks
Obesity is a major risk factor for serious health problems including coronary heart disease, high blood pressure, diabetes, hypertension, etc. Though an overweight person also faces a risk of these medical problems but an obese is more susceptible to them.
Obese people are at high risk of depression and other social problems. Obesity is an excess of body fat sufficient to shorten one's life span and make one susceptible to a greater amount of illness than would occur if the body weight were normal. Calorific imbalance that results often develops from a combination of genetic and environmental factors. A combination of an excessive nutrient intake and a sedentary lifestyle are the main cause for the rapid acceleration of obesity.
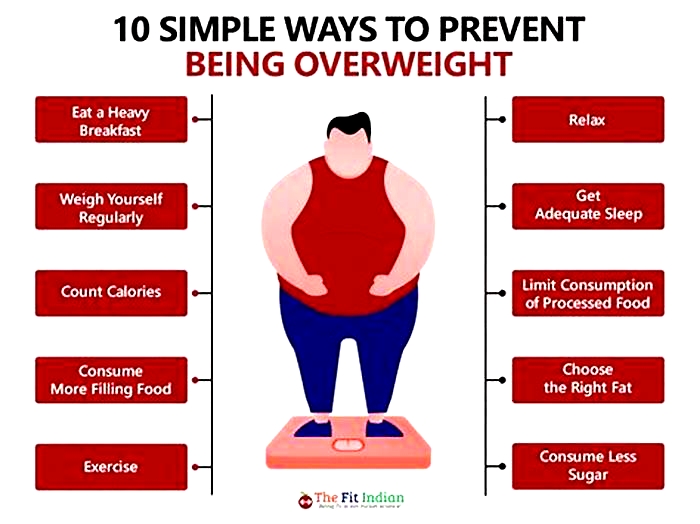
Control
The safest and most effective way to lose weight in both cases is to reduce calories (balanced diet) and increase physical activity. In excess cases of obesity a person can undergo surgery.
References
Overweight and obesity: How do they compare?
While overweight and obesity are similar weight-related conditions, they also have differences. If a person has a higher body weight, the doctor will typically evaluate their body mass index (BMI) to detect if they have overweight or obesity.
According to the
The cause of overweight and obesity may be multifactorial. This includes eating patterns, lack of sleep, low physical activity, certain medications, genetics, and family history.
Healthcare professionals screen adults for overweight and obesity using body mass index (BMI). This is a measure of body fat based on someones height and weight. The formula takes a persons body weight in kilograms divided by their square of height in meters. It is expressed in units of kg/m.
A doctor will consider other related measures, such as waist circumference, to evaluate a persons risk of having overweight and obesity.
This article explores the comparison between overweight and obesity.
The United Kingdoms National Health Service (NHS) notes that obesity is a complex condition with multiple causes.
Excess calories
If a person continually consumes more high fat or high sugar foods than they burn, the excess calories
According to the NHS, the following dietary lifestyle may affect a persons risk of having overweight and obesity:
- eating large amounts of fast or processed foods
- consuming large amounts of alcohol
- drinking a lot of sweetened drinks
- engaging in comfort eating
Sedentary lifestyle
Not getting enough physical activity alongside consuming high calorie, low nutrient foods and beverages
The CDC recommends
Genetics
Genetic variations
Medications
A
Medical conditions
Certain medical conditions can also contribute to weight gain, which can lead to overweight and obesity. These conditions include:
There are various ways doctors can recommend for treating overweight and obesity. These include lifestyle changes, medications, and surgery.
Lifestyle changes
A healthcare professional can recommend some lifestyle modifications to improve well-being and prevent the severity of overweight or obesity. This may include:
Learn about eating a balanced diet.
Behavioral weight-loss programs
In a behavioral weight-loss program, a healthcare professional or dietitian works closely with a person to identify habits affecting their body weight and develop a personalized lifestyle modification plan to help them lose weight. Typically, this plan is reviewed with the healthcare professional or dietitian every
Medications
The doctor may prescribe weight loss medications if eating and physical activity are not significantly benefiting a persons weight loss. Some effective weight loss medications
Surgery
A doctor
An individual should discuss all benefits and risks of surgery with a doctor.
The following are some common questions about overweight and obesity.
How does overweight cause obesity?
Usually, being overweight is a risk factor for obesity. If the BMI of a person who is overweight increases to 30 or higher, they will have obesity.
Can you be both overweight and obese?
A person can be both overweight and obese. Obesity is a form of overweight and is where BMI is 30 or higher.
What are the common causes of obesity?
- eating habits
- sedentary lifestyle
- genetics
Although overweight and obesity are similar, they are different conditions.
Healthcare professionals diagnose overweight if a person has a BMI range of 2530 and obesity if they have a BMI of 30 or higher.
According to medical experts, overweight and obesity may be due to several reasons, including low physical activity, high fat and high calorie diet, certain medications or medical conditions, and genetics.
Overweight and obesity may cause health complications such as stroke, osteoarthritis, high blood pressure, and mental health conditions. Treatments include lifestyle changes, medications, and surgery.
Defining Adult Overweight & Obesity
1Garrow, J.S. & Webster, J., 1985. Quetelets index (W/H2) as a measure of fatness. Int. J. Obes., 9(2), pp.147153.
2Freedman, D.S., Horlick, M. & Berenson, G.S., 2013. A comparison of the Slaughter skinfold-thickness equations and BMI in predicting body fatness and cardiovascular disease risk factor levels in children. Am. J. Clin. Nutr., 98(6), pp.141724.
3Wohlfahrt-Veje, C. et al., 2014. Body fat throughout childhood in 2647 healthy Danish children: agreement of BMI, waist circumference, skinfolds with dual X-ray absorptiometry. Eur. J. Clin. Nutr., 68(6), pp.66470.
4Steinberger, J. et al., 2005. Comparison of body fatness measurements by BMI and skinfolds vs dual energy X-ray absorptiometry and their relation to cardiovascular risk factors in adolescents. Int. J. Obes., 29(11), pp.13461352.
5Sun, Q. et al., 2010. Comparison of dual-energy x-ray absorptiometric and anthropometric measures of adiposity in relation to adiposity-related biologic factors. Am. J. Epidemiol., 172(12), pp.14421454.
6Lawlor, D.A. et al., 2010. Association between general and central adiposity in childhood, and change in these, with cardiovascular risk factors in adolescence: prospective cohort study. BMJ, 341, p.c6224.
7Flegal, K.M. & Graubard, B.I., 2009. Estimates of excess deaths associated with body mass index and other anthropometric variables. Am. J. Clin. Nutr., 89(4), pp.12131219.
8Freedman, D.S. et al., 2009. Relation of body mass index and skinfold thicknesses to cardiovascular disease risk factors in children: the Bogalusa Heart Study. Am. J. Clin. Nutr., 90(1), pp.210216.
9Willett, K. et al., 2006. Comparison of bioelectrical impedance and BMI in predicting obesity-related medical conditions. Obes. (Silver Spring), 14(3), pp.480490.
Overweight versus Obese: Different Risk and Different Management
Body mass index (BMI) is a widely accepted calculation of adiposity in human beings. Standard BMI ranges () signify categories of excess weight that have been linked to risk for a variety of health conditions, including hyperlipidemia, diabetes mellitus, hypertension, sleep apnea, stroke, and cardiovascular disease. Recently, the accuracy with which the categories indicate risk of death has come into question. Similarly, the question of whether a given BMI represents the same degree of risk across racial and ethnic groups is being considered. The answers to these questions might affect how providers counsel patients about weight loss.
TABLE I.
Standard Body Mass Index Categories
Body Mass Index and Mortality Rates
Two large meta-analyses by Flegal and associates1,2 examined the association between BMI and risk of death. The first1 involved 97 studies that used standard BMI categories in reporting hazard ratios for all-cause death. A hazard ratio of 1.0 suggests that a condition or factor imparts no increased risk of death when compared with a reference (lowest-risk) group. Values less than 1.0 suggest less risk than in the reference group. Values greater than 1.0 suggest greater risk than in the reference group. The systematic review encompassed 2.88 million individuals and 270,000 deaths. Using standard BMI categories, the study suggests that, in considering the impact of BMI status on risk of death, only stage 2 obesityBMI 35results in an increased risk ().1 The 2nd large study,2 a meta-analysis of 8 large observational studies, involved 5.8 million individuals and 582,000 deaths. This study, like the previous one, used hazard ratios to describe risk of death, but it subdivided standard normal-weight and overweight BMI categories into smaller ranges. In women, BMI values between 23 and 25 were identified as the reference group; however, there was no significantly increased risk of death in women with values between 20 (normal-weight category) and 27 (low-overweight category). The study did not subdivide stage I obesity into smaller ranges, and its findings suggest an increased risk of death for women whose BMI is 30.2
TABLE II.
Summary Hazard Ratios of All-Cause Mortality for Overweight and Obesity, Compared with Normal Weight1
Body Mass Index, Mortality Rates, and Special Populations
Although data appear to support the need to reevaluate concerns about mortality risk at low levels of excess weight, it is worth considering whether these findings apply to individuals with comorbid conditions that increase the risk of cardiovascular disease. In a study of individuals with type 2 diabetes mellitus (a known cardiovascular disease equivalent), hazard ratios for death are higher at all BMI levels greater than 25.3 If an individual has diabetes, any excess weight increases the risk of death.
Evidence suggests variable effects of excess weight on different ethnic populations. In a study examining the effect of BMI on life expectancy in women, black women were found to lose fewer years of life with increasing BMI, when compared with white women. In addition, the impact of excess weight on life expectancy did not result until white women were at least class II obese (BMI 30) and black women were at least class III obese (BMI 40).4 A separate study explored the risk of developing traditional cardiovascular disease risk factors in terms of BMI and racial group. Each increase in BMI above 25 resulted in a larger proportional increase in prevalence of cardiovascular disease risk factors (diabetes mellitus, hypertension, and low high-density-lipoprotein cholesterol levels), in whites when compared with blacks.5 Again, this study suggests that there might be different effects of BMI on individuals from different ethnic and racial groups.
Clinical Implications
Although there is growing evidence that all-cause risk of death does not increase for women who are overweightor black women who are class I obesewithout comorbid conditions, this does not mean that weight management can be ignored in these groups. Clinicians should instead consider varying levels of weight-management intensity tailored to individual patients and their risk (). Adults who do nothing to manage their weight will gain 1 to 2 pounds per year. For individuals without comorbid conditions who are overweight, or who in some cases are mildly obese, providers may do best to stress the importance of weight-gain prevention. A medium-intensity intervention in overweight and class I obese black women was successful in preventing weight gain. A menu of measurable health practices (walking 10,000 steps/d, watching <2 hr television/d, avoiding sugar-sweetened beverages, avoiding fast food, eating breakfast every day, and avoiding late-night eating) was used, in addition to regular weighing, to help patients with self-monitoring.6 For individuals with comorbid conditions, especially pre-diabetes or diabetes, or class II obesity, providers should strongly encourage weight loss for risk reduction. Intensive lifestyle interventions like the Diabetes Prevention Program (7% weight loss and 150 min/wk physical activity) or the use of weight-loss medications (phentermine, orlistat, phentermine/topiramate combination, and lorcaserin) might be appropriate in higher-risk groups.
TABLE III.
Approach to Weight Management