Should labs eat once or twice a day
How Often Should You Feed a Labrador? (Dog Routines Matter)
Labrador Feeding Schedules
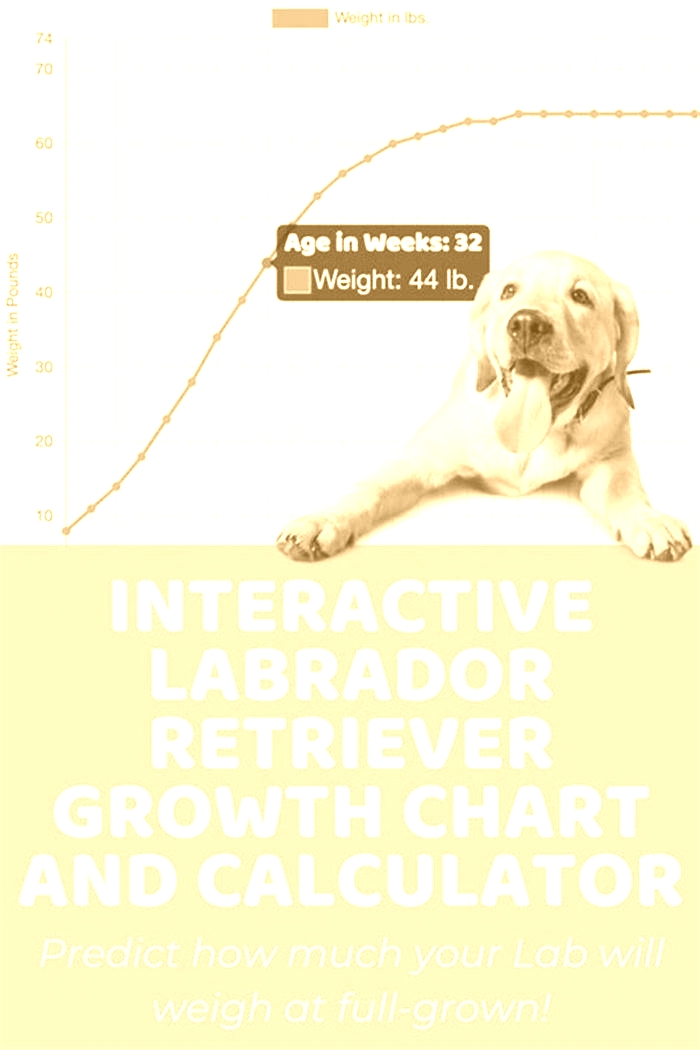
Labrador adults, like most dogs, work well when fed on a schedule. Twice per day is the standard as it allows the dog to eat and digest properly.
Puppies will require more frequent feedings, though, as they expend far more energy and smaller stomachs to hold their needed food.
If you have a Labrador that gets a lot of exercise, you may want to consider feeding them less food more often, as they will likely feel hungry sooner.
Feed Your Labrador At Least Every 12 hours
Remember that your Labrador shouldn't go more than12 hourswithout food to avoid nausea. Age, size, and the food's nutritional content should determine the amount of food given.
Whatever the frequency, it's crucial for your puppy or dog to have a regular feeding schedule. Disrupting this can cause digestive problems that are unpleasant for the dog and the owner.
According to Veterinary Centers of America, dogs are creatures of habit thatneed the security and predictability of their feeding routine. In addition, keeping the feeding schedule consistent helps your pet cope with other changes that may occur within the household.
Lastly, never free-feed a Labrador. While Labradors may not technically eat themselves to death, they can certainly make themselves sick if you let them decide how much and how often to eat.
What to Do If Your Lab Doesn't Finish Its Meal
Some dogs don't eat their entire portion during mealtime, which is okay as long as it's normal behavior for your Lab. This is especially true while you're trying to establish a set routine for when your Lab will eat its meals.
Feed Your Lab Less Food More Frequently
If you find that your Labrador isn't interested in eating the entire meal in a single sitting, you can add more mealtime if it works for your schedule. To do this, you should take the whole day's meal portion and divide it evenly into the desired number of meals.
For example, if you feed your dog 1 cups in the morning and night, that's three cups total for the day. If you add an extra mealtime, you should serve 1 cup at each of the three meals.
In other words, adding another mealtime doesn't mean that you add more food intake to the day's total.
Use Interactive Food Dispensers
Another option is to use an interactive toy to dispense the food, which may help to keep your dog's attention for the entire mealtime.
For example, I recommend buying Outward Hound Store'sNina Ottosson Interactive Puzzle Game. It is an excellent option to hide food or treats. This particular item is perfect for a Labrador because it will allow your pet to use its intelligence to solve a puzzle and problem-solve while being rewarded with the kibble hidden inside.
Although it isn't a good option for every Lab's mealtime, it is an idea for a pup that loses interest in their food before finishing.
How Much to Feed a Labrador
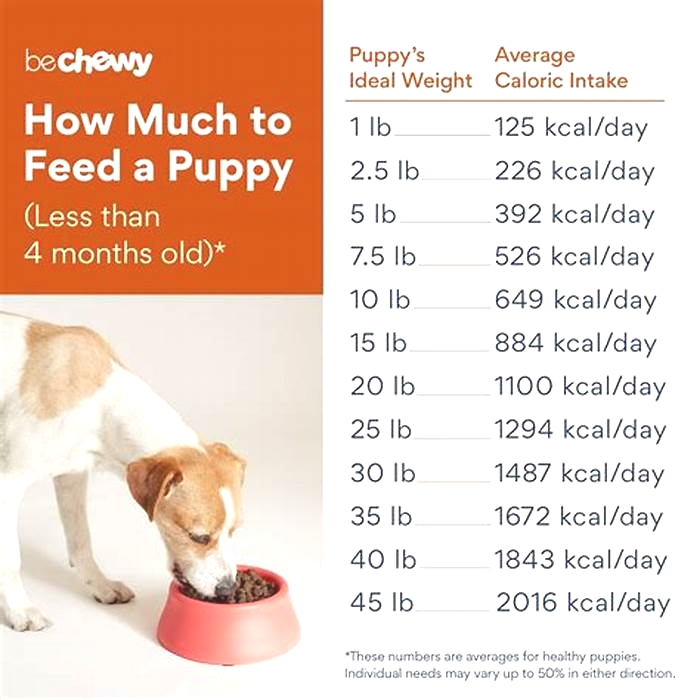
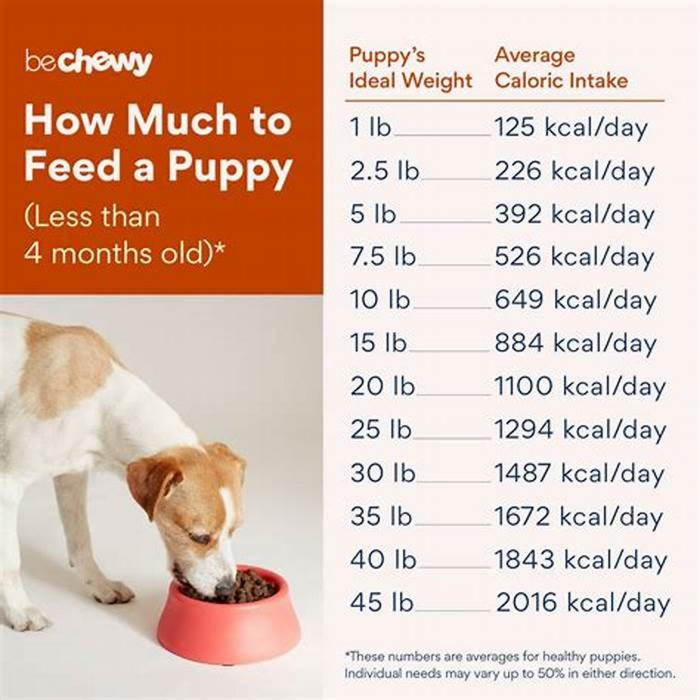
Your Lab's portions at each meal should depend on a few different factors. First of all, you need to know if your pup is currently at ahealthy weight.
Dogs are typically considered overweight at 15% over their ideal weight and obese if they're 30% over their ideal weight. So the best thing to do in this case is to ask your veterinarian if your Lab is at a healthy weight.
If your Lab is not at an ideal weight, you'll need to talk to your vet and amend the feeding plan. You may also consider a specialized food designed to help your dog reach the appropriate weight.
Your Labrador's activity level will also impact how much he needs to eat each day. It's always a good idea to consult the feeding guide on your dog food and your veterinarian's advice to make an informed decision.
Labrador Feeding Schedule Examples
To give you an idea of a standard feeding schedule and meal plan, here is a chart based on the feeding recommendation from Royal Canin's Labrador Retriever dry puppy food:
| Adult Target Weight: | 2 months | 3 months | 6 months | 12 months | 14 months |
|---|---|---|---|---|---|
| 57 lbs. (26 kg) | 2 cups | 3 cups | 3 cups | 3 cups | 3 cups |
| 70 lbs. (32 kg) | 2 cups | 3 cups | 4 cups | 3 cups | 3 cups |
| 88 lbs. (40 kg) | 2 cups | 3 cups | 5 cups | 4 cups | 4 cups |
*2-5 months: split into three equal portions per day.*6-15 months: split into two equal portions per day.
Here are the feeding recommendations for an adult Labrador Retriever with an average activity level:
| Dog's Weight: | Amount Per Day (in cups) | 3 months | 6 months | 12 months | 14 months |
|---|---|---|---|---|---|
| 57 lbs. (26 kg) | 4 | 3 cups | 3 cups | 3 cups | 3 cups |
| 66 lbs. (30 kg) | 4 | 3 cups | 4 cups | 3 cups | 3 cups |
| 75 lbs. (34 kg) | 5 | 3 cups | 5 cups | 4 cups | 4 cups |
| 84 lbs. (38 kg) | 5 | ||||
| 97 lbs. (44 kg) | 6 |
*Split the daily amount into two equal feedings, morning and evening.
Food specifically for Labradors
If you like the idea of breed-specific dog food formulas, I highly recommend an adult formula like theRoyal Canin Labrador Retriever Adult Breed. For a puppy formula, I recommendRoyal Canin Labrador Retriever Puppy Breed. Both are great because they are specially designed for the nutritional demands of a purebred Lab.
The kibble is shaped to encourage slower eating and more careful chewing. I also like that the food has nutrients to support a healthy coat and joints.
Sudden Changes in a Labrador's Eating Habits
Because dogs are so routine-oriented, a sudden change in their eating habits can be a warning sign. In that case, you should contact your veterinarian to ensure that there isn't an underlying issue.
Conclusion
Most adult Labradors should eat twice per day, while puppies will eat less food more frequently until they are around six months old. Be sure to follow the guidance printed on the package of the food you are feeding your dog. Every dog food has different ingredients and recommended portion sizes.
Only adjust the recommended feeding schedule if your vet advises something different due to medical or dietary reasons. If you are unsure how much to feed your Lab, consult your vet for appropriate guidance.
Metformin (Oral Route)
Description and Brand Names
Drug information provided by: Merative, Micromedex
US Brand Name
- Fortamet
- Glucophage
- Glucophage XR
- Glumetza
- Riomet
- Riomet ER
Canadian Brand Name
- ACT metFORMIN
- AG-metFORMIN - Blackberry
- AG-metFORMIN - Unflavored
- APO-metFORMIN
- APO-metFORMIN ER
- AURO-metFORMIN
- AVA-metFORMIN
- Bio-metFORMIN
- Dom-metFORMIN
Descriptions
Metformin is used to treat high blood sugar levels that are caused by a type of diabetes mellitus or sugar diabetes called type 2 diabetes. With this type of diabetes, insulin produced by the pancreas is not able to get sugar into the cells of the body where it can work properly. Using metformin alone, with a type of oral antidiabetic medicine called a sulfonylurea, or with insulin, will help to lower blood sugar when it is too high and help restore the way you use food to make energy.
Many people can control type 2 diabetes with diet and exercise. Following a specially planned diet and exercise will always be important when you have diabetes, even when you are taking medicines. To work properly, the amount of metformin you take must be balanced against the amount and type of food you eat and the amount of exercise you do. If you change your diet or exercise, you will want to test your blood sugar to find out if it is too low. Your doctor will teach you what to do if this happens.
Metformin does not help patients who have insulin-dependent or type 1 diabetes because they cannot produce insulin from their pancreas gland. Their blood glucose is best controlled by insulin injections.
This medicine is available only with your doctor's prescription.
This product is available in the following dosage forms:
- Tablet, Extended Release
- Suspension, Extended Release
- Tablet
- Solution
- Tablet, Extended Release, 24 HR
Before Using
In deciding to use a medicine, the risks of taking the medicine must be weighed against the good it will do. This is a decision you and your doctor will make. For this medicine, the following should be considered:
Allergies
Tell your doctor if you have ever had any unusual or allergic reaction to this medicine or any other medicines. Also tell your health care professional if you have any other types of allergies, such as to foods, dyes, preservatives, or animals. For non-prescription products, read the label or package ingredients carefully.
Pediatric
Appropriate studies performed to date have not demonstrated pediatric-specific problems that would limit the usefulness of metformin oral solution, extended-release oral suspension, and tablets in children 10 to 16 years of age. However, safety and efficacy of metformin extended-release tablets in the pediatric population have not been established.
Geriatric
Although appropriate studies on the relationship of age to the effects of metformin have not been performed in the geriatric population, geriatric-specific problems are not expected to limit the usefulness of metformin in the elderly. However, elderly patients are more likely to have age-related kidney problems, which may require caution in patients receiving metformin. This medicine is not recommended in patients 80 years of age and older who have kidney problems.
Breastfeeding
There are no adequate studies in women for determining infant risk when using this medication during breastfeeding. Weigh the potential benefits against the potential risks before taking this medication while breastfeeding.
Drug Interactions
Although certain medicines should not be used together at all, in other cases two different medicines may be used together even if an interaction might occur. In these cases, your doctor may want to change the dose, or other precautions may be necessary. When you are taking this medicine, it is especially important that your healthcare professional know if you are taking any of the medicines listed below. The following interactions have been selected on the basis of their potential significance and are not necessarily all-inclusive.
Using this medicine with any of the following medicines is usually not recommended, but may be required in some cases. If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines.
- Abiraterone Acetate
- Acetazolamide
- Alogliptin
- Aspirin
- Bexagliflozin
- Bictegravir
- Brinzolamide
- Bupropion
- Capmatinib
- Chloroquine
- Chlorpropamide
- Cimetidine
- Ciprofloxacin
- Dasabuvir
- Delafloxacin
- Diatrizoate
- Dichlorphenamide
- Dofetilide
- Dolutegravir
- Dorzolamide
- Enoxacin
- Ethiodized Oil
- Fedratinib
- Fexinidazole
- Gatifloxacin
- Gemifloxacin
- Glimepiride
- Glipizide
- Glyburide
- Grepafloxacin
- Hydroxychloroquine
- Insulin
- Insulin Aspart, Recombinant
- Insulin Bovine
- Insulin Degludec
- Insulin Detemir
- Insulin Glargine, Recombinant
- Insulin Glulisine
- Insulin Lispro, Recombinant
- Iodipamide
- Iodixanol
- Iohexol
- Iopamidol
- Iopanoic Acid
- Iopromide
- Iothalamate
- Iotrolan
- Ioversol
- Ioxaglate
- Ipodate
- Isavuconazole
- Lanreotide Acetate
- Levofloxacin
- Levoketoconazole
- Liraglutide
- Lomefloxacin
- Methazolamide
- Metrizamide
- Moxifloxacin
- Nateglinide
- Norfloxacin
- Octreotide Acetate
- Ofloxacin
- Ombitasvir
- Paritaprevir
- Pasireotide Diaspartate
- Pioglitazone
- Pramlintide
- Ranolazine
- Repaglinide
- Semaglutide
- Sitagliptin
- Somatrogon-ghla
- Sotagliflozin
- Sparfloxacin
- Tafenoquine
- Thioctic Acid
- Tolazamide
- Tolbutamide
- Topiramate
- Trovafloxacin
- Vandetanib
- Zonisamide
Using this medicine with any of the following medicines may cause an increased risk of certain side effects, but using both drugs may be the best treatment for you. If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines.
- Acebutolol
- Atenolol
- Betaxolol
- Bisoprolol
- Bitter Melon
- Carteolol
- Carvedilol
- Celiprolol
- Colesevelam
- Esmolol
- Fenugreek
- Glecaprevir
- Glucomannan
- Goldenseal
- Guar Gum
- Hydrastis
- Isocarboxazid
- Labetalol
- Levobunolol
- Linezolid
- Methylene Blue
- Metipranolol
- Metoprolol
- Nadolol
- Nebivolol
- Oxprenolol
- Ozanimod
- Patiromer
- Penbutolol
- Phenelzine
- Pibrentasvir
- Pindolol
- Practolol
- Procarbazine
- Propranolol
- Psyllium
- Rasagiline
- Rifampin
- Safinamide
- Selegiline
- Sotalol
- Timolol
- Tirzepatide
- Tranylcypromine
- Verapamil
Other Interactions
Certain medicines should not be used at or around the time of eating food or eating certain types of food since interactions may occur. Using alcohol or tobacco with certain medicines may also cause interactions to occur. The following interactions have been selected on the basis of their potential significance and are not necessarily all-inclusive.
Other Medical Problems
The presence of other medical problems may affect the use of this medicine. Make sure you tell your doctor if you have any other medical problems, especially:
- Alcohol, excessive use or
- Underactive adrenal glands or
- Underactive pituitary gland or
- Undernourished condition or
- Weakened physical condition or
- Any other condition that causes low blood sugarPatients with these conditions may be more likely to develop low blood sugar while taking metformin.
- Anemia (low levels of red blood cells) or
- Vitamin B12 deficiencyUse with caution. May make these conditions worse.
- Congestive heart failure, acute or unstable or
- Dehydration or
- Heart attack, acute or
- Hypoxemia (decreased oxygen in the blood) or
- Kidney disease or
- Liver disease or
- Sepsis (blood poisoning) or
- Shock (low blood pressure, blood circulation is poor)A rare condition called lactic acidosis can occur. Talk with your doctor if you have concerns about this.
- Diabetic ketoacidosis (ketones in the blood) or
- Kidney disease, severe or
- Metabolic acidosis (extra acids in the blood) or
- Type 1 diabetesShould not be used in patients with these conditions.
- Fever or
- Infection or
- Surgery or
- TraumaThese conditions may cause temporary problems with blood sugar control and your doctor may want to treat you with insulin.
Proper Use
This medicine usually comes with a patient information insert. Read the information carefully and make sure you understand it before taking this medicine. If you have any questions, ask your doctor.
Carefully follow the special meal plan your doctor gave you. This is a very important part of controlling your condition, and is necessary if the medicine is to work properly. Also, exercise regularly and test for sugar in your blood or urine as directed.
Metformin should be taken with meals to help reduce stomach or bowel side effects that may occur during the first few weeks of treatment.
Swallow the tablet or extended-release tablet whole with a full glass of water. Do not crush, break, or chew it.
While taking the extended-release tablet, part of the tablet may pass into your stool after your body has absorbed the medicine. This is normal and nothing to worry about.
Measure the oral liquid with a marked measuring spoon, oral syringe, or medicine cup. The average household teaspoon may not hold the right amount of liquid.
Use the supplied dosing cup to measure the mixed extended-release oral suspension. Ask your pharmacist for a dosing cup if you do not have one.
Use only the brand of this medicine that your doctor prescribed. Different brands may not work the same way.
You may notice improvement in your blood glucose control in 1 to 2 weeks, but the full effect of blood glucose control may take up to 2 to 3 months. Ask your doctor if you have any questions about this.
Dosing
The dose of this medicine will be different for different patients. Follow your doctor's orders or the directions on the label. The following information includes only the average doses of this medicine. If your dose is different, do not change it unless your doctor tells you to do so.
The amount of medicine that you take depends on the strength of the medicine. Also, the number of doses you take each day, the time allowed between doses, and the length of time you take the medicine depend on the medical problem for which you are using the medicine.
- For type 2 diabetes:
- For oral dosage form (extended-release tablets):
- Adults
- Metformin alone (Fortamet): At first, 1000 milligrams (mg) once a day taken with the evening meal. Your doctor may increase your dose if needed until your blood sugar is controlled. However, the dose is usually not more than 2500 mg per day.
- Metformin alone (Glucophage XR): At first, 500 mg once daily with the evening meal. Your doctor may increase your dose if needed until your blood sugar is controlled. However, the dose is usually not more than 2000 mg per day.
- Metformin alone (Glumetza): At first, 500 mg once a day taken with the evening meal. Then, your doctor may increase your dose if needed until your blood sugar is controlled. However, the dose is usually not more than 2000 mg per day.
- Metformin with a sulfonylurea: Your doctor will determine the dose of each medicine.
- Metformin with insulin: At first, 500 mg once a day. Then, your doctor may increase your dose by 500 mg every week if needed until your blood sugar is controlled. However, the dose is usually not more than 2500 mg per day.
- ChildrenUse and dose must be determined by your doctor.
- Adults
- For oral dosage form (extended-release suspension):
- AdultsAt first, 5 milliliters (mL) once a day taken with the evening meal. Your doctor may increase your dose by 5 mL weekly if needed until your blood sugar is controlled. However, the dose is usually not more than 20 mL per day.
- Children 10 to 16 years of ageAt first, 5 mL once a day taken with the evening meal. Your doctor may increase your dose by 5 mL weekly if needed until your blood sugar is controlled. However, the dose is usually not more than 20 mL per day.
- Children younger than 10 years of ageUse and dose must be determined by your doctor.
- For oral dosage form (solution):
- Adults
- Metformin alone: At first, 5 milliliters (mL) two times a day, or 8.5 mL once a day with meals. Your doctor may increase your dose if needed until your blood sugar is controlled. However, the dose is usually not more than 25.5 mL per day.
- Metformin with a sulfonylurea: Your doctor will determine the dose of each medicine.
- Metformin with insulin: At first, 5 mL once a day. Your doctor may increase your dose if needed until your blood sugar is controlled. However, the dose is usually not more than 25 mL per day.
- Children 10 to 16 years of ageAt first, 5 mL two times a day with meals. Your doctor may increase your dose if needed until your blood sugar is controlled. However, the dose is usually not more than 20 mL per day.
- Children younger than 10 years of ageUse and dose must be determined by your doctor.
- Adults
- For oral dosage form (tablets):
- Adults
- Metformin alone: At first, 500 milligrams (mg) two times a day taken with the morning and evening meals, or 850 mg a day taken with the morning meal. Your doctor may increase your dose if needed until your blood sugar is controlled. Later, your doctor may want you to take 500 or 850 mg two to three times a day with meals. However, the dose is usually not more than 2550 mg per day.
- Metformin with a sulfonylurea: Your doctor will determine the dose of each medicine.
- Metformin with insulin: At first, 500 mg a day. Your doctor may increase your dose by 500 mg every week if needed until your blood sugar is controlled. However, the dose is usually not more than 2500 mg per day.
- Children 10 to 16 years of ageAt first, 500 mg two times a day taken with the morning and evening meals. Your doctor may increase your dose if needed until your blood sugar is controlled. However, the dose is usually not more than 2000 mg per day.
- Children younger than 10 years of ageUse and dose must be determined by your doctor.
- Adults
- For oral dosage form (extended-release tablets):
Missed Dose
If you miss a dose of this medicine, take it as soon as possible. However, if it is almost time for your next dose, skip the missed dose and go back to your regular dosing schedule. Do not double doses.
Storage
Store the medicine in a closed container at room temperature, away from heat, moisture, and direct light. Keep from freezing.
Keep out of the reach of children.
Do not keep outdated medicine or medicine no longer needed.
Ask your healthcare professional how you should dispose of any medicine you do not use.
Precautions
It is very important that your doctor check your or your child's progress at regular visits, especially during the first few weeks that you take this medicine. Blood and urine tests may be needed to check for unwanted effects.
This medicine may interact with the dye used for an X-ray or CT scan. Your doctor should advise you to stop taking it before you have any medical exams or diagnostic tests that might cause less urine output than usual. You may be advised to start taking the medicine again 48 hours after the exams or tests if your kidney function is tested and found to be normal.
Make sure any doctor or dentist who treats you knows that you are using this medicine. You may need to stop using this medicine several days before having surgery or medical tests.
It is very important to carefully follow any instructions from your health care team about:
- AlcoholDrinking alcohol may cause severe low blood sugar. Discuss this with your health care team.
- Other medicinesDo not take other medicines unless they have been discussed with your doctor. This especially includes nonprescription medicines such as aspirin, and medicines for appetite control, asthma, colds, cough, hay fever, or sinus problems.
- CounselingOther family members need to learn how to prevent side effects or help with side effects if they occur. Also, patients with diabetes may need special counseling about diabetes medicine dosing changes that might occur with lifestyle changes, such as changes in exercise or diet. Counseling on birth control and pregnancy may be needed because of the problems that can occur in pregnancy for patients with diabetes.
- TravelKeep a recent prescription and your medical history with you. Be prepared for an emergency as you would normally. Make allowances for changing time zones and keep your meal times as close as possible to your usual meal times.
- In case of emergencyThere may be a time when you need emergency help for a problem caused by your diabetes. You need to be prepared for these emergencies. It is a good idea to wear a medical identification (ID) bracelet or neck chain at all times. Also, carry an ID card in your wallet or purse that says that you have diabetes and a list of all of your medicines.
Under certain conditions, too much metformin can cause lactic acidosis. The symptoms of lactic acidosis are severe and quick to appear, and usually occur when other health problems not related to the medicine are present and are very severe, such as a heart attack or kidney failure. Symptoms of lactic acidosis include abdominal or stomach discomfort, decreased appetite, diarrhea, fast or shallow breathing, a general feeling of discomfort, severe muscle pain or cramping, and unusual sleepiness, tiredness, or weakness.
If symptoms of lactic acidosis occur, you should get immediate emergency medical help.
This medicine may cause some premenopausal women who do not have regular monthly periods to ovulate. This can increase the chance of pregnancy. If you are a woman of childbearing potential, you should discuss birth control options with your doctor.
This medicine may cause hypoglycemia (low blood sugar). This is more common when this medicine is taken together with certain medicines. Low blood sugar must be treated before it causes you to pass out (unconsciousness). People feel different symptoms of low blood sugar. It is important that you learn which symptoms you usually have so you can treat it quickly. Talk to your doctor about the best way to treat low blood sugar.
Hyperglycemia (high blood sugar) may occur if you do not take enough or skip a dose of your medicine, overeat or do not follow your meal plan, have a fever or infection, or do not exercise as much as usual. High blood sugar can be very serious and must be treated right away. It is important that you learn which symptoms you have in order to treat it quickly. Talk to your doctor about the best way to treat high blood sugar.
High blood sugar may occur if you do not exercise as much as usual, have a fever or infection, do not take enough or skip a dose of your diabetes medicine, or overeat or do not follow your meal plan.
Side Effects
Along with its needed effects, a medicine may cause some unwanted effects. Although not all of these side effects may occur, if they do occur they may need medical attention.
Check with your doctor immediately if any of the following side effects occur:
More common
- Abdominal or stomach discomfort
- cough or hoarseness
- decreased appetite
- diarrhea
- fast or shallow breathing
- fever or chills
- general feeling of discomfort
- lower back or side pain
- muscle pain or cramping
- painful or difficult urination
- sleepiness
Less common
- Anxiety
- blurred vision
- chest discomfort
- cold sweats
- coma
- confusion
- cool, pale skin
- depression
- difficult or labored breathing
- dizziness
- fast, irregular, pounding, or racing heartbeat or pulse
- feeling of warmth
- headache
- increased hunger
- increased sweating
- nausea
- nervousness
- nightmares
- redness of the face, neck, arms, and occasionally, upper chest
- seizures
- shakiness
- slurred speech
- tightness in the chest
- unusual tiredness or weakness
Rare
- Behavior change similar to being drunk
- difficulty with concentrating
- drowsiness
- lack or loss of strength
- restless sleep
- unusual sleepiness
Some side effects may occur that usually do not need medical attention. These side effects may go away during treatment as your body adjusts to the medicine. Also, your health care professional may be able to tell you about ways to prevent or reduce some of these side effects. Check with your health care professional if any of the following side effects continue or are bothersome or if you have any questions about them:
More common
- Acid or sour stomach
- belching
- bloated
- excess air or gas in the stomach or intestines
- full feeling
- heartburn
- indigestion
- loss of appetite
- metallic taste in the mouth
- passing of gas
- stomachache
- stomach upset or pain
- vomiting
- weight loss
Less common
- Abnormal stools
- bad, unusual, or unpleasant (after) taste
- change in taste
- difficulty with moving
- discoloration of the fingernails or toenails
- flu-like symptoms
- joint pain
- rash
- sneezing
- stuffy or runny nose
- swollen joints
Other side effects not listed may also occur in some patients. If you notice any other effects, check with your healthcare professional.
Call your doctor for medical advice about side effects. You may report side effects to the FDA at 1-800-FDA-1088.
Portions of this document last updated: March 01, 2024
Original article: https://www.mayoclinic.org/drugs-supplements/metformin-oral-route/proper-use/DRG-20067074