Is it better to be underweight or obese

What are the risks of being underweight?
If a person is underweight, their body may not be getting the nutrients it needs to build healthy bones, skin, and hair. Related symptoms or signs can include osteoporosis, anemia, feeling tired, and more.
While some people may have a genetic background or a medical illness that prevents them from putting on weight, there are interventions doctors can recommend to help a person gain weight.
In this article, we look at ways to tell if you are underweight, causes, treatments, and when to see a doctor.
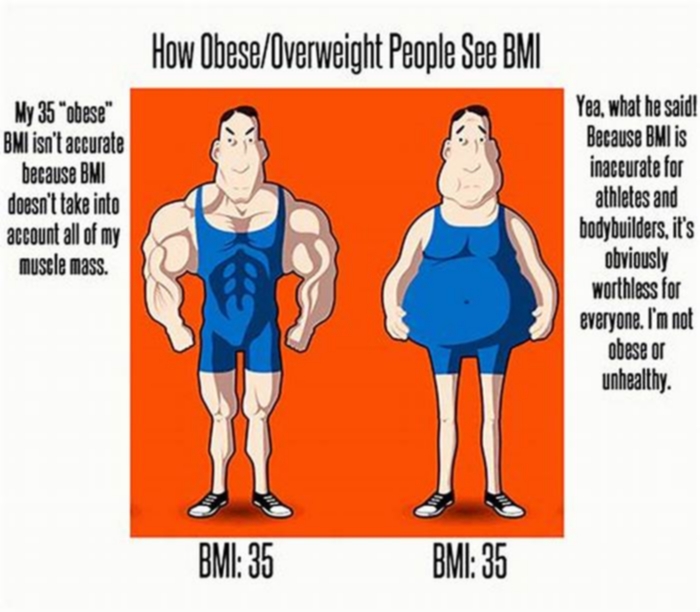
The Centers for Disease Control and Prevention (CDC) recommend people use a body mass index (BMI) to calculate if they are underweight, at a healthy weight, or overweight.
Using the BMI is considered a good measure of a persons weight because it compares their weight to their height. For example, a 170-pound person may not be overweight if they are very tall but could be overweight if they are very short.
A person can calculate their BMI by visiting the CDCs
- Underweight: less than 18.5
- Normal/healthy weight: 18.5 to 24.9
- Overweight: 25.0 to 29.9
- Obese: 30 or higher
These calculations may be slightly inaccurate for a person who is an elite or endurance athlete whose body has a significant amount of muscle. This is because muscle weighs more than fat.
Being underweight can cause health problems, just as being overweight can.
Not all people who are underweight experience adverse side effects or symptoms from being underweight. However, some people, experience the following symptoms related to being underweight:
- Osteoporosis. According to a
2016 study , being underweight increases a womans risk of osteoporosis, which is where the bones are brittle and more prone to breaking. - Skin, hair, or teeth problems. If a person does not get enough nutrients in their daily diet, they may display physical symptoms, such as thinning skin, hair loss, dry skin, or poor dental health.
- Getting sick frequently. If a person does not get enough energy from their diet to maintain a healthy body weight, they may also not be getting enough nutrients to fight off infections. As a result, a person may get sick more frequently, and common illnesses, such as a cold, can last longer than they usually would.
- Feeling tired all the time. Calories are a measurement of the energy a particular food can give a person. Not getting enough calories to maintain a healthy weight can make a person feel fatigued.
- Anemia. A person who is underweight is more likely to have low blood counts, known as anemia, which causes dizziness, headaches, and fatigue.
- Irregular periods. Women who are underweight may not have regular periods, they may find menstruation stops, or an adolescents first period may be delayed or absent. Irregular or absent menstruation can cause infertility.
- Premature births. According to a study published in
An International Journal of Obstetrics & Gynaecology , a woman who is pregnant and underweight is at a higher risk for pre-term labor, which means having a baby before 37 weeks. - Slow or impaired growth. Young people need nutrients to grow and develop healthy bones. Being underweight and not getting enough calories could mean a person may not develop as expected. Doctors call this a failure to thrive.
According to a study published in the journal
There are a variety of reasons why a person may be underweight. Sometimes, multiple underlying causes may be related. Causes of being underweight include:
- Family history. Some people have a naturally low BMI due to physical characteristics that run in their family.
- A high metabolism. If a person has a high metabolism, they may not gain much weight even when eating high-energy foods.
- Frequent physical activity. Athletes or people who engage in high levels of physical activity, such as runners, may burn significant amounts of calories that result in low body weight.
- Physical illness or chronic disease. Some disease types can cause regular nausea, vomiting, and diarrhea, making it difficult to gain weight. Other conditions may decrease a persons appetite, so they do not feel like eating. Examples include cancer, diabetes, thyroid disorders, and digestive conditions, such as Crohns disease or ulcerative colitis.
- Mental illness. Poor mental health can affect a persons ability to eat, including depression, anxiety, obsessive-compulsive disorder (OCD), and eating disorders, such as anorexia and bulimia. Each of these conditions can affect a persons body image and appetite.
A doctor can help a person identify the cause of their low BMI and recommend a treatment plan that allows them to gain weight healthfully.
If a person is underweight, there are various healthful weight-gain methods that they can try.
A person can gain weight by following a healthful diet that incorporates nutritious calorie-dense foods. A doctor may recommend a person tries a specific diet for weight gain or refer them to a dietitian, who can help a person develop a diet plan that works for them.
Some key components of a diet for weight gain may include:
- Adding snacks. High-protein and whole-grain carbohydrate snacks can help a person gain weight. Examples include peanut butter crackers, protein bars, trail mix, pita chips and hummus, or a handful of almonds.
- Eating several small meals a day. Sometimes a person may be underweight because they cannot tolerate eating large meals. Instead, a person can eat several small meals throughout the day.
- Incorporating additional foods. A person can add calorie-dense food sources to their existing diet, such as putting slivered almonds on top of cereal or yogurt, sunflower or chia seeds on a salad or soup, or nut butter on whole-grain toast.
- Avoiding empty calories. Eating high-calorie foods may cause a person to gain weight, but they also have excess fats that could affect a persons heart and blood vessels. A person should avoid foods that are high in sugar and salt.
Doctors may also prescribe anti-nausea medications or appetite stimulants to help a person who is underweight gain weight whenever possible. Doctors will usually only prescribe these treatments when at-home treatments have not worked.
A person should see their doctor if they have tried to gain weight but have not been able to. Anyone who is experiencing any effects of ill health due to being unable to gain weight, such as missed periods or infertility, should also see a doctor.
If a person struggles with mental illness or an eating disorder, it is essential they seek professional help. Unfortunately, a person may not always recognize their behavior is a problem.
Some of the symptoms associated with eating disorders include:
- secretive behavior
- sudden, unexplained weight loss
- refusal to attend family or social events
- appearing fatigued
- refusing to eat in front of others
If a person has these symptoms, their friends or family members should encourage them to seek professional help from a doctor or therapist.
A person who is underweight may be at an increased risk of developing complications, including bone, teeth, and fertility problems.
A person should aim to maintain a healthy BMI. Working with a medical professional can help a person achieve and sustain a healthy weight.
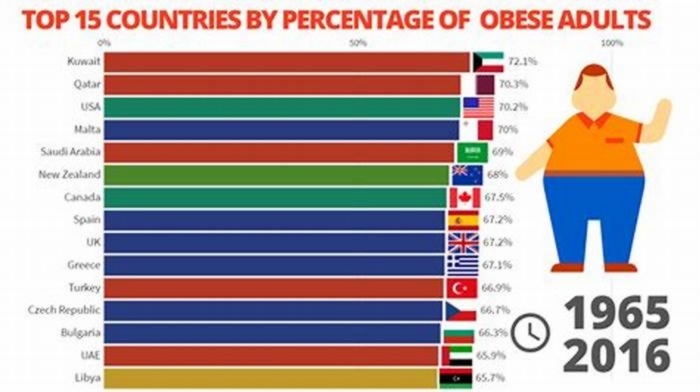
Evidence about the health effects of being underweight is inconclusive and often contradictory. Being underweight is associated with higher all-cause mortality[1,2]. The effects seem to be more pronounced for men than for women[1]. After controlling for other covariates such as smoking, underweight women have significant reductions in mortality while underweight men have higher mortality[3]. Although obesity increases the risk of cardiovascular diseases such as heart failure, among persons who already have heart failure, outcomes are better for obese persons than for lean ones[4]. Furthermore, for patients with chronic conditions undergoing treatments such as haemodialysis, higher body weight is associated with lower mortality risks[5]. Being underweight is associated with higher all-cause mortality, and increased risks for inpatient care for circulatory diseases[1]. However,breast cancer patients who are overweight or obese have higher mortality riskthan lean individual[6].
There are indications of similarities in health outcomes of underweight and obese individuals. Relative to having healthy body weight, being obese or underweight is associated with a higher risk of death among female breast cancer patients[7]. Lung transplant candidates who are underweight or obese have a higher risk of post-transplant mortality than recipients with a healthy weight[8].
Given the inconclusive evidence and few studies about the effects of being underweight, it is important to examine this issue further to gather evidence that will guide effective intervention creation and implementation.
Study ObjectivesThe main study question was: Is being underweight as bad for your health as being obese? Related questions are: Relative to individuals with healthy body weights (18.5 BMI < 25), what is the health status of those who are underweight (BMI < 18.5)? Relative to the health status of individuals who are obese (30 BMI < 35 Class1 obese; 35 BMI < 40 Class2 obese; and 40 BMI Class3 obese), what is the health status of those who are underweight?
Study Methods
Study modelThe study applied a household health production framework from health economics which posits that, the household produces health using household, individual and environmental inputs[9]. The basic model used in previous studies[10-13], can be represented by the following health production function:
Hi = f(Ii, Ei) (1)Where: the subscript i denotes the individual as the unit of analysis; H is a vector depicting health output; I is a set of individual and household variables (inputs) and E represents environmental inputs. Researchers have applied this framework in studies of various health-related phenomena such as effects of prenatal care on birth weights[14]; household production and demand for health inputs and their effects on birth weights[15] effects of childhood and education on health[16]; the impact of maternal smoking on child neurodevelopment[8] and the relationship between household production, fertility and child mortality[17]. Within the health production framework, body weight classes are inputs in the production of general, physical, and mental health. Based on the household health production process represented by equation 1 above the econometric model we use in multivariate analysis of general health (GH) utilizes the following equation:
GHi = f(Di, Si, Bi, Hi, Ei) (2)Where: D represents demographic factors; S is socioeconomic status (SES); B is health behaviors; H is stock of health capital, E are environmental factors such as access to care. This equation represents the analysis model used to address study question three. Health status is measured as self-assessed general health status, and the number days within a 30-day period that an individual experienced poor physical health.
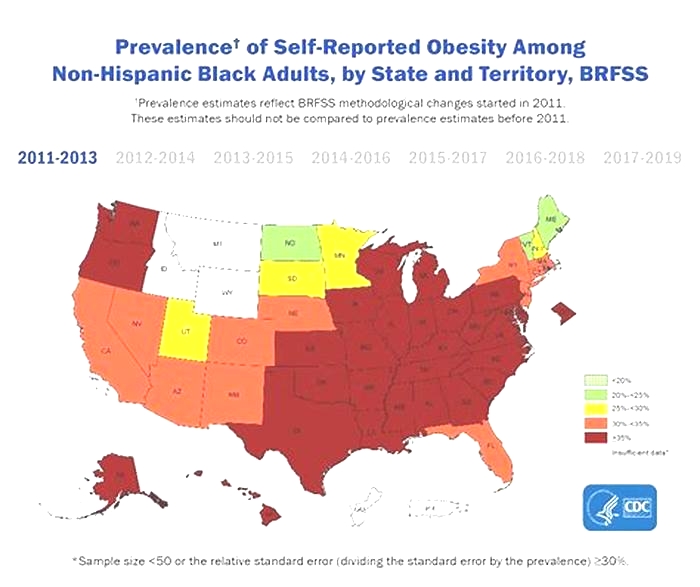
Data Source and study variablesThe study data source was the 2012 Behavioral Risk Factor Surveillance System (BRFSS) survey. BRFSS is an annual nationwide telephone survey of non-institutionalized adults conducted by the CDC in collaboration with state health departments[18]. The survey is based on a multistage cluster design that uses random-digit dialing to select samples that are representative of the US population. Itincludes questions about health behaviors, health status, socioeconomic status variables, environmental variables and othersthat affect health. The study sample is drawn from all states in the US.
Dependent variablesThe 2012 BRFSS survey had questions about individual self-assessed general health (GH) status: Would you say that in general your health is 1. Excellent, 2. Very good, 3. Good, 4. Fair, or 5. Poor? Responses to this question were coded one (1) for excellent, very good or good health and zero (0) for fair or poor health. Other BRFSS questions quantified poor health experiences in number of days of poor health within a 30-day period: Now thinking about your physical health, which includes physical illness and injury, for how many days during the past 30 days was your physical health not good? Responses to these questions provided quantitative measures of the individuals health status.
Independent variablesData about body weight were derived from responses to two BRFSS questions: About how much do you weigh without shoes? About how tall are you without shoes? Responses to these questions were used to calculate respondents body mass index (BMI), which was then coded into six body weight classes: BMI < 18.5 is underweight; 18.5 BMI < 25 is healthy weight; 25 BMI< 30 is overweight; 30 BMI < 35 is Class1 obese; 35 BMI< 40 is Class2 and BMI 40 is Class 3 obese.
BRFSS data included the individuals demographics such asage, ethnicity, sex, marital and veteran status. There was dataon educational attainment, income, home-ownership, employment, educational levels and access to personal cell-phones. Other data wereused as surrogate measures of household climate, including number of dependent children, whether the household was female-headed with no adult males or male-headed with no adult females present.
Measures of individual health behavior included tobacco and alcohol use, participation in physical exercise, the use of seatbelts in automobiles, vaccination status, and health screenings such as HIV-tests. BRFSS also provided data about access to care and health capital. We measured access to careusing three variables: having health insurance and personal doctors and inability to access care due to high costs of care. Measures of individual health capital stock weredisability status and whether the respondent had ever been diagnosed with chronic health conditions.
Disability was measured from responses to two BRFSS questions: Are you limited in any way in any activities because of physical, mental, or emotional problems? Do you now have any health problem that requires you to use special equipment, such as a cane, a wheelchair, a special bed, or a special telephone? Responses to these questions were coded one (1) for yes and zero (0) for no.
Data about chronic health conditions were derived from responses to BRFSS survey question: Has a doctor, nurse, or other health professional EVER told you that you had any of the following: heart attack also called a myocardial infarction, angina or coronary heart disease, stroke, asthma, skin cancer, other types of cancer, chronic obstructive pulmonary disease (COPD), arthritis, depressive disorder, kidney disease, trouble seeing, diabetes? Responses to these questions were coded one (1) for yes and zero (0) for no. It is important to note that BRFSS defines arthritis to include rheumatoid arthritis, gout, lupus, or fibromyalgia and COPD to include emphysema or chronic bronchitis. Depressive disorders include depression, major depression, dysthymia or minor depression.
We measured oral health using responses to the BRFSS question: How many of your permanent teeth have been removed because of tooth decay or gum disease? Include teeth lost to infection, but do not include teeth lost for other reasons, such as injury or orthodontics. Responses indicating tooth loss were coded one (1) and those with no tooth loss were coded zero (0). We also measured eyesight using responses to the question: How much difficulty, if any, do you have in recognizing a friend across the street? Responses indicating visual difficulties were coded one (1) and those with no visual difficulties were coded zero (0).
Analysis methodsTo test the study hypothesis, Students T test (t-test) and Chi-Square test of independence ( test) were utilized to determine the statistical significance of the differences in health, disability and prevalence of chronic health conditions across the body weight classes. We applied testson differences in categorical variables and t-tests for differences in the number of days respondents experienced poor health.
Multivariate analysis estimated the likelihood of good general health as represented in equations 2 above. To set a control group, we tested the assumption that there was no general health status difference between the healthy body-weight and the overweight classes. This assumption was based on examination of the data which indicated general health status differences between the healthy body weight class and the overweight to be very small. For example, the difference in the number of days of poor health in a 30-day period was 0.29 days. Setting alpha = 0.05, we testedthe statistical significance of the general health status differences between these two body weight classes and found them to be statistically insignificant. Based on this finding we used these two bodyweight classes (which includeindividuals with 18.5 BMI < 30) as the control in multivariate analysis. This analysis enabled the study to measure the effects of being underweight or obese while controlling for other health production factors.
Results
Table 1 displays study sample distribution by body weight class and the average number of days they experience poor health within a 30-day period. The largest group (66.2%) includes individuals with healthy weight (32%) or overweight (34.2%). The smallest group (7,803 people or 1.6% of the sample) were underweight, while 27% were obese.
On average, individuals with a healthy body weight or who are overweight experienced approximately four days of poor physical health within a 30-day period. Class3 obese individuals experiencedthe largest number of days (about nine days) of poor physical health. Underweight individuals and those who are Class2 obese experienced about six days while those who are Class1 obese experienced five days of poor physical health in a 30-day period.
Table 1: Sample distribution of weight classes and average number of days in poor physical health within a 30-day period.
| Body weight class | N | % of Sample Total | Mean Days in poor physical health |
|---|---|---|---|
| Underweight (BMI < 18.5) | 7,803 | 1.6 | 6.22 |
| Healthy weight (18.5 BMI < 25) | 151,985 | 32.0 | 3.57 |
| Overweight (25 BMI < 30) | 162,768 | 34.2 | 3.86 |
| Class1 Obese (30 BMI < 35) | 79,839 | 16.8 | 5.1 |
| Class2 Obese (35 BMI < 40) | 29,429 | 6.2 | 6.48 |
| Class3 Obese (40 BMI) | 18,388 | 3.9 | 8.91 |
| Total | 450,212 | 94.6 | |
| Unknown* | 25,475 | 5.4 |
*BMI could not be determined because the individual didnt answer questions about their weight or height.
Table 2: Results of t-tests of differences in days of poor physical health in a 30-day period between underweight and other five body-weight classes.
| Body Weight Class | Mean Days | Mean Difference | T-Statistic | N |
|---|---|---|---|---|
| Under weight (BMI < 18.5) | 6.22 | 0 | 7803 | |
| Healthy weight (18.5 BMI < 25) | 3.57 | 2.65 | 27.39a | 156615 |
| Over weight (25 BMI < 30) | 3.86 | 2.36 | 23.69 a | 167311 |
| Class1 Obese (30 BMI < 35) | 5.1 | 1.12 | 9.74b | 85765 |
| Class2 Obese (35 BMI < 40) | 6.48 | -0.26 | 1.87 | 36392 |
| Class3 Obese(40 BMI) | 8.91 | -2.69 | 17.23a | 25529 |
ap < 0.000, bp < 0.01
Table 2 displays results of t-tests of mean-differences (in number of days of poor physical health) between underweight individuals and individuals in the other five body-weight classes. Underweight individuals experience 2.65 days more of poor physical health than those with healthy body weight and 2.36 days more than those who are overweight. These differences are statistically significant (p < 0.000). Individuals with Class1 obesity experience 1.12 days less of poorphysical health than those who are underweight and this difference is also statistically significant (p < 0.01). The difference between underweight and Class 2 obese individuals is very small (0.26 days) and statistically insignificant. Individuals with Class3 obesity experience 2.69 more days of poor physical health than those who are underweight. This difference is also statistically significant (p < 0.000). These results suggest that being underweight might havea similar effect on physical health as being Class 2 obese.
Table 3 displays percentages of individuals in good health, those diagnosed with chronic health conditions, those with disabilities, and those using assistive devices. The proportions are displayed for each body weight class, and the proportion average for the study sample.
Table 3: Distribution of individuals in each body weight group by health condition.
| Health Condition | Percent of total number of individuals in each body weight class in good health and those diagnosed with the specified chronic health condition | ||||||
|---|---|---|---|---|---|---|---|
| Under-Weight | Healthy weight | Over weight | Class1 Obese | Class2 Obese | Class3 Obese | Sample Average | |
| Self-assessed good health | |||||||
| Good general Health | 73.5 | 85.4 | 83.1 | 76.3 | 68.2 | 55.5 | 80.4 |
| Good physical health | 55.5 | 65.9 | 64.7 | 58.0 | 50.5 | 40.7 | 61.8 |
| Disability | |||||||
| Has Disability | 29.8 | 19.4 | 22.2 | 29.6 | 37.2 | 49.9 | 24.8 |
| Uses Assistive Devices | 15.2 | 8.2 | 9.5 | 13.5 | 19.5 | 30.2 | 11.4 |
| Diagnosed chronic condition | |||||||
| Heart attack | 6.4 | 4.7 | 6.4 | 7.5 | 8.1 | 8.5 | 6.2 |
| Angina or coronary heart disease | 5.4 | 4.6 | 6.5 | 7.8 | 8.9 | 10.0 | 6.4 |
| Stroke | 5.5 | 3.6 | 4.1 | 4.5 | 5.1 | 5.4 | 4.1 |
| COPD | 15.5 | 6.8 | 6.8 | 9.0 | 11.9 | 16.7 | 8.1 |
| Asthma | 12.9 | 10.6 | 11.1 | 14.5 | 19.4 | 26.0 | 12.7 |
| Diabetes | 4.4 | 5.5 | 11.2 | 19.1 | 26.9 | 34.8 | 12.5 |
| Kidney disease | 3.5 | 2.6 | 3.0 | 3.8 | 5.1 | 6.0 | 3.3 |
| Arthritis | 29.3 | 27.5 | 33.5 | 41.3 | 47.1 | 54.0 | 34.5 |
| Depressive disorder | 20.2 | 15.7 | 16.5 | 21.4 | 27.0 | 35.3 | 18.6 |
| Skin cancer | 9.0 | 9.2 | 9.2 | 7.9 | 7.0 | 5.2 | 8.7 |
| Other cancer | 11.3 | 9.0 | 9.3 | 9.4 | 9.1 | 9.2 | 9.2 |
| Lost at least one permanent tooth | 53.0 | 46.4 | 53.9 | 59.0 | 61.5 | 65.1 | 53.2 |
| Poor eye-sight | 20.5 | 15.7 | 16.3 | 19.1 | 22.1 | 27.5 | 17.5 |
Comparisons of proportions of underweight individuals to average sample proportions indicate that the underweight self-assessed good health is lower, and their disability proportions are higher than the sample average. With the exception of angina, arthritis, and diabetes, the proportion of underweight individuals diagnosed with chronic conditions is much higher than the sample average.
A comparison between the underweight and healthy weight classes indicates that the underweight have poorer self-assessed general and physical health, higher disability and greater proportions of diagnosed chronic conditions. These numbers seem to suggest that on the average, underweight individuals might have poorer health than individuals with healthy body weights.
Comparisons of overweight and underweight classes show that the underweight class has poorer self-assessed general and physical health, and higher disability. The underweight class also has greater proportions diagnosed with chronic health conditions except for heart attack, angina, diabetes, arthritis, diabetes, and skin cancer where the proportions for overweight individuals are higher or equal to the proportions for the underweight class. The proportion of underweight individuals diagnosed with heart-attack is 6.4% exactly equal to the proportion for individuals who are overweight. The proportions of overweight individuals diagnosed with angina,diabetes, and arthritis are higher than proportions of underweight individuals diagnosed with these conditions. These results suggest that on the average, the underweight are less healthy than the overweight.
Compared to Class1 obese, the underweight have lower proportions with good self-assessed general and physical health, suggesting that they are less healthy. Although they have similar disability (as shown by their similar disability proportions) the proportion of underweight individuals using assistive devices is higher than for Class1 obese denoting that the underweight have more severe disability. The proportions diagnosed with depressive disorders or kidney disease is similar and both are above the sample average. However, the underweight class has smaller proportions of individuals diagnosed with diabetes, heart attack, angina, asthma and arthritis. From these results one might infer that on the average, the underweight have worse or similar health to Class1 obese except for the five chronic conditions.
Comparisons of proportions of the underweight with Class2 obese show that Class2 obese has poorer self-assessed general and physical health, greater disability, and higherproportions diagnosed with asthma, arthritis, depressive disorder, kidney disease, poor sight, oral health and diabetes. However, Class2 obese is similar to or better than the underweight in proportions diagnosed with stroke, skin and other cancers and COPD.
Compared to Class3 obese, the underweight fare better in all measures applied with some exceptions. The proportion of underweight individuals diagnosed with stroke (5.5%) is only slightly higher the proportion for individuals who are Class3 obese (5.4%) and is much higher than the sample average (4.1%). The underweight also have higher proportions of skin and other cancer than Class3 obese.
Table 4 displays results of tests of proportional differences between the underweight and the other five bodyweight classes. The test statistics indicate that all health differences (except skin cancer) between the underweight and the healthy weight classes are statistically significant. The health of the underweight class is significantly poorer than the health of the healthy weight class except for diabetes. The healthy weight class has higher proportions diagnosed with diabetes than the underweight class. The difference in skin cancer diagnosis is statistically insignificant.
The test statistics of the health differences between underweight and the overweight classes show the differences to be statistically significant except for proportions diagnosed with heart attack, skin cancer and oral health. The overweight class has significantly greater proportions diagnosed with of angina, arthritis, and diabetes than the underweight. For all other measures of health (including general health, physical health, disability, and cancer) the health of the underweight class is significantly worse than that of the overweight.
Differences between obese Class1 and the underweight class are statistically significant except disability and kidney disease diagnosis. However, the difference for disability measured in terms of the use of assistive devices was statistically significant (p < 0.000). This finding suggests that the underweight class has a proportionately greater need for assistive devices than Class1 obese. Measured in terms of general and physical health and in proportions diagnosed with stroke, skin cancer, other cancer, COPD, and poor sight, the health status of Class1 obese is better than that of underweight class. However, Class1 obese has significantly (p < 0.000) higher proportions diagnosed with diabetes, arthritis, heart attack, angina, and oral health measured as loss of at least one permanent tooth.
Differences between Class2 obese and the underweight class are statistically significant except for proportions diagnosed with stroke. The numbers show that Class2 obese has significantly worse health than the underweight class. However, the underweight class has significantly greater proportions diagnosed with skin and other cancers that Class2 obese. These findings are similar to findings about the differences between the underweight class and Class3 obese.
Table 4: Results of tests of differences in health status of Underweight individuals and of the other five body weight classes.
| Health Status & Health Capital | Healthy Weight | Overweight | Class1 Obese | Class2 Obese | Class3 Obese |
|---|---|---|---|---|---|
| Self-assessed good health | |||||
| Good General Health | 805.95a | 475.9a | 30.22a | 83.29 a | 742.7a |
| Good Physical Health | 353.77a | 277.23a | 17.92a | 60.76a | 484.66a |
| Disability | |||||
| Has a Disability | 496.57a | 242.91a | 0.18 | 141.43a | 876.16a |
| Uses Assistive Devices | 460.41a | 275.02a | 16.99a | 74.08a | 633.73a |
| Diagnosed Chronic Conditions | |||||
| Heart Attack | 46.24a | 0.009 | 11.27b | 24.21a | 31.16a |
| Angina | 9.3b | 15.21 a | 60.34a | 99.56a | 146.56a |
| Stroke | 77.24a | 37.05a | 15.54a | 2.11 | 0.089 |
| COPD | 848.05a | 831.47a | 347.52a | 72.34a | 5.75c |
| Asthma | 41.06a | 24.81a | 14.49a | 173.82a | 537.24a |
| Diabetes | 17.334a | 350.20a | 1048.04a | 1810.59a | 2647.48a |
| Kidney Disease | 20.37a | 4.78* | 2.59 | 37.75a | 69.60a |
| Arthritis | 11.99b | 57.94 a | 422.58a | 788.04a | 1332.18a |
| Depressive Disorder | 112.48a | 74.27a | 5.61c | 149.15a | 584.68a |
| Skin Cancer | 0.26 | 0.13 | 13.14a | 37.31a | 134.92a |
| Other Cancer | 44.23a | 34.46a | 27.65a | 34.72a | 25.20a |
| Lost at least one permanent tooth | 125.56a | 2.50 | 101.95 | 183.18a | 330.81a |
| Has poor eye-sight | 123.64a | 93.71a | 8.11b | 9.16b | 142.99a |
ap < 0.000, bp < 0.01, cp < 0.05
Table 5 displays multivariate analysis results. These are results of logistic regression analysis estimating the likelihood of good general health while controlling for other relevant determinants of health such as demographics, SES and other variables.
Table 5: Results of Logistic Regression Estimating the Effects of Body-weight on the Likelihood of Good General Health.
| B | Wald | Sig. | Exp(B) (Odds-ratio) | 95% C.I. for EXP(B) | ||
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Demographics | ||||||
| Female | .205 | 111.403 | .000 | 1.227 | 1.181 | 1.274 |
| Latino/a | -.750 | 876.537 | .000 | .473 | .450 | .497 |
| Young | .190 | 37.348 | .000 | 1.209 | 1.138 | 1.285 |
| Veteran | .018 | .764 | .382 | 1.018 | .978 | 1.060 |
| Household climate | ||||||
| Dependent Children | .025 | 9.020 | .003 | 1.025 | 1.009 | 1.042 |
| No Adult Women | -.008 | .134 | .714 | .992 | .950 | 1.036 |
| No Adult Men | .076 | 18.421 | .000 | 1.078 | 1.042 | 1.116 |
| Body Weight | ||||||
| Underweight | -.422 | 78.664 | .000 | .656 | .597 | .720 |
| Class1 obese | -.079 | 23.180 | .000 | .924 | .895 | .954 |
| Class2 obese | -.258 | 124.151 | .000 | .773 | .738 | .809 |
| Class3 obese | -.469 | 283.023 | .000 | .626 | .593 | .661 |
| SES | ||||||
| Unemployed | -.549 | 908.067 | .000 | .578 | .557 | .599 |
| Education Level | .277 | 1619.134 | .000 | 1.319 | 1.302 | 1.337 |
| Income | .116 | 913.777 | .000 | 1.123 | 1.115 | 1.132 |
| Has personal Cellphone | .250 | 265.778 | .000 | 1.283 | 1.246 | 1.323 |
| Health Behavior | ||||||
| Non-Smoker | .098 | 51.435 | .000 | 1.103 | 1.074 | 1.133 |
| Current-drinker | .317 | 510.815 | .000 | 1.373 | 1.335 | 1.411 |
| Pneumonia shot | -.130 | 82.833 | .000 | .878 | .854 | .903 |
| Physical Ex. | .551 | 1614.952 | .000 | 1.735 | 1.689 | 1.783 |
| Seat belt always | .043 | 5.779 | .016 | 1.044 | 1.008 | 1.081 |
| HIV-tested | -.073 | 21.665 | .000 | .930 | .901 | .959 |
| Access to care | ||||||
| Insured | .0372 | .493 | .114 | 1.038 | .991 | 1.088 |
| Has personal doctor | -.088 | 13.707 | .000 | .916 | .875 | .960 |
| Cost-Barred | -.451 | 498.888 | .000 | .637 | .612 | .663 |
| Health Capital | ||||||
| Heart Attack | -.449 | 348.896 | .000 | .639 | .609 | .669 |
| Angina | -.637 | 756.635 | .000 | .529 | .505 | .553 |
| Stroke | .726 | 197.198 | .000 | .689 | .654 | -.372 |
| Asthma | -.163 | 74.934 | .000 | .849 | .818 | .881 |
| Other cancer | -.551 | 885.270 | .000 | .576 | .556 | .597 |
| COPD | -.672 | 1101.029 | .000 | .511 | .491 | .532 |
| Arthritis | -.377 | 722.944 | .000 | .686 | .667 | .705 |
| Depression | -.340 | 468.316 | .000 | .712 | .690 | .734 |
| Kidney | -.630 | 478.086 | .000 | .532 | .503 | .563 |
| Poor Sight | -.411 | 730.264 | .000 | .663 | .644 | .683 |
| Diabetes | -.729 | 1977.307 | .000 | .482 | .467 | .498 |
| Disability | -1.125 | 5802.094 | .000 | .325 | .315 | .334 |
| Assistive Devices | -.553 | 990.782 | .000 | .575 | .556 | .596 |
| Model fit | R = .466 | = 87333.31 | Accurate Prediction = 86.2% | N = 253806 |
The logistic regression results show that relative to having a healthy weight, being underweight or Class1-3 obese has a negative and statistically significant (p < 0.000) effect on the likelihood of good general health. Coefficient sizes indicate that being underweight has a larger negative effect on the likelihood of good health than being Class1 or Class 2 obese but a slightly smaller effect than Class3 obese. Other factors with statistically significant and negative effects on the likelihood of good health are: being unemployed or Latino/a, and having poor health capital stock as indicated by diagnosis of chronic health conditions such as heart attacks, angina, stroke, asthma and cancer. Factors that relate positively with the likelihood of good health are educational attainment, income, social support (measured by having access to a cellphone), having good health behavior (such as not smoking and engaging in physical exercise) being female and being young.
Discussion
The results seem to suggest that being underweight has a significant effect on health, disability and incidence of chronic health conditions. The results show that health effects of body weight differ across the six bodyweight classes. The underweight self-assessed good health is lower and their disability proportions are higher than the sample average. Proportions of underweight individuals diagnosed with chronic conditions are much higher than the sample average except for angina, arthritis, diabetes, and kidney disease. The underweight appear to have lower incidences of these conditions.
The health of the underweight appears to be worse than the health status of those with healthy body weight, overweight, and Class1 obese. Being underweight appears to have a larger negative effect on the likelihood of good general health than being Class1 obese. Classes 2 and 3 obese have significantly worse health than the underweight class. However, the underweight class has significantly greater proportions diagnosed with skin and other cancers than Classes 2 and 3 obese.
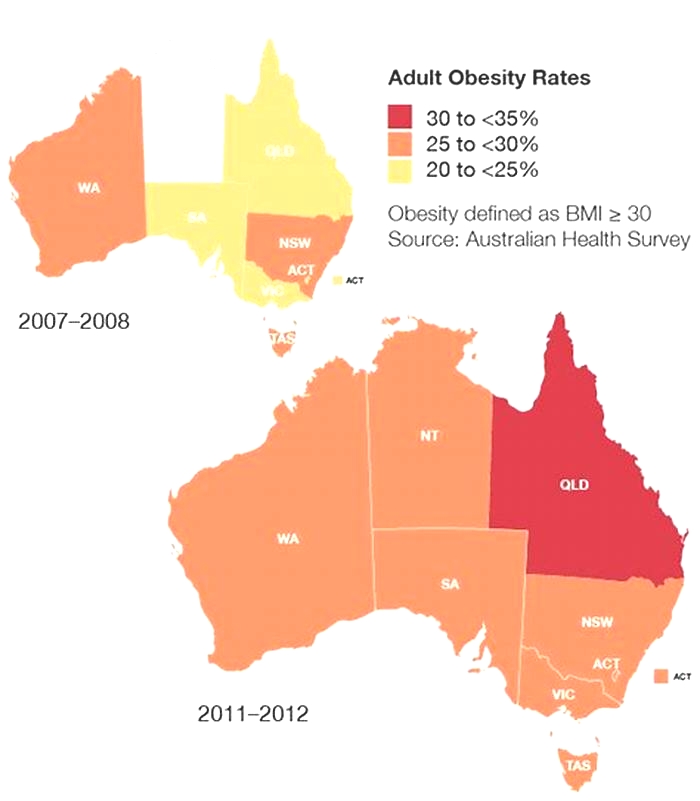
Before drawing any conclusions from these results, it is important to note that the interpretation of these results should be cognizant of the strengths and weakness of the BRFSS data. These dataare cross-sectional, representing a single snapshot in time. Consequently, no causality can be established. Furthermore, the data are from the US and the results might not necessarily generalize to other populations with different social, economic, and political environments or different health systems.
An important strength of the BRFSS is that CDCs strong quality control over survey questions ensures that data collected are comparable across all states in the US. The survey questions have been used and improved upon consistently since 1984. Over time BRFSS has developed a computer-assisted-telephone-interviewing system which improves data collection speed and reduces survey costs. Because it is an ongoing survey, it provides useful means of tracking trends on prevalence of self-reported asthma/adult asthma history, cardiovascular disease, diabetes, health risk factors and behaviors. BRFSS data is self-reported, therefore, it has the advantage of gathering information that is only available to the individual.
A major weakness of the BRFSS is that it excludes individuals who are institutionalized or have no telephones. Individuals with no telephones tend to be low-income with higher health risks. This fact suggests that BRFSS data might understate health risks. BRFSS data come from self-reported information. Individuals tend to underreport their risky behaviors especially those that are socially undesirable or illegal. Therefore, BRFSSs data might underreport such behaviors. Other weakness include possible biases resulting from less than ideal response rates common to telephone surveys, inaccurate recall by those responding to the survey, cultural biases, language barriers, or inadequate health knowledge might result in inaccurate responses to the survey. Any generalizations or conclusions must be read within the context of these data strengths and weaknesses.
Conclusion and Implications
These results suggest that being underweight is as bad (or worse) for health as being class1 obese. It is slightly better than being Class2 or 3 obese. The results also show differences in health status and diagnosis across the six weight classes. Therefore, it is important to study the effect of body weight on health in a more targeted manner using specific bodyweight classes. The targeted examination might lead to more targeted and relevant interventions. It is as important for public health to consider and examine underweight as Class 1 obese. Although individuals with obesity Classes2 and 3 have worse effects on health than being underweight, for specific conditions such as cancer, it might be more urgent to examine being underweight. Because of the statistically significant health differences across the six body weight classes, it is important for studies to examine the relationship between body weight and health with specific body weight classes. Instead of treating obesity as one group, it might be more useful to examine it as three specific conditions.
References
- 1. Seidell, J.C., Verschuren, W.M., van Leer, E.M., et al. Overweight, underweight, and mortality. A prospective study of 48,287 men and women. (1996) Arch Intern Med 156(9): 958-963.Pubmed || Crossref || Others
- 2. Ringbck, W.G., Eliasson, M., Rosn, M. Underweight, overweight and obesity as risk factors for mortality and hospitalization. (2008) Scand J Public Health 36(2): 69-176. Pubmed || Crossref || Others
- 3. Wndell, P.E., Carlsson, A.C., Theobald, H. The association between BMI value and long-term mortality. (2009) Int J Obes (Lond) 33(5): 577-582. Pubmed || Crossref || Others
- 4. Oga, E.A., Eseyin, O.R. (2016) The Obesity Paradox and Heart Failure: A Systematic Review of a Decade of Evidence. (2016) J Obes. Pubmed || Crossref || Others
- 5. Chazot, C., Gassia, J.P., Di Benedetto, A., et al. Is there any survival advantage of obesity in Southern European haemodialysis patients? (2009) Nephrol Dial Transplant 24(9): 2871-2876. Pubmed || Crossref || Others
- 6. Chan, D.S., Vieira, A.R., Aune, D., et al. Body mass index and survival in women with breast cancer-systematic literature review and meta-analysis of 82 follow- up studies. (2014) Ann Oncol 25(10): 1901-1914. Pubmed || Crossref || Others
- 7. Kawai, M., Tomotaki, A., Miyata, H., et al. Body mass index and survival after diagnosis of invasive breast cancer: a study based on the Japanese National Clinical Database-Breast Cancer Registry. (2016) Cancer Med 5(6): 1328-1340.Pubmed || Crossref || Others
- 8. Upala, S., Panichsillapakit, T., Wijarnpreecha, K., et al. Underweight and obesity increase the risk of mortality after lung transplantation: a systematic review and meta-analysis. (2016) Transpl Int 29(3): 285-296. Pubmed || Crossref || Others
- 9. Grossman, M. On the concept of health capital and the demand for health. (1972) The J Political Econ 80(2): 223255.Pubmed || Crossref || Others
- 10. Grossman, M., Joyce, T. Unobservables, Pregnancy Resolutions, and Birth-Weight Production Functions in New York City. (1990) J Political Econ 98(5): 9831007.Pubmed || Crossref || Others
- 11. Behrman, J.R., Rosenzweig, M.R. Returns to birth weight. The Review of Economics and Statistics (2004) 86(2): 586601.Pubmed || Crossref || Others
- 12. Wehby, G.L., Murray, J.C., Castilla, E.E., et al. Prenatal care effectiveness and utilization in Brazil. (2009) Health Policy Plan 24(3): 175-188. Pubmed || Crossref || Others
- 13. Mityakov, S., Mroz, T. Economic theory as a guide for the specification and interpretation of empirical health production functions. (2013). Pubmed || Crossref || Others
- 14. Rosenzweig, M.R., Schultz, T.P. Estimating a Household Production Function: Heterogeneity, the Demand for Health Inputs, and Their Effects on Birth Weight. (1983) J Political Econ 91(5): 723-746.Pubmed || Crossref || Others
- 15. Conti, G., Heckman, J.J., Urzua, S. Early endowments, education and health. (2011) Becker Friedman Institute Research Repository. Pubmed || Crossref || Others
- 16. Wehby, G.L., Prater, K., McCarthy, A.M., et al. (2011) The impact of maternal smoking during pregnancy on early child neurodevelopment. 5(2): 207-254.Pubmed || Crossref || Others
- 17. About the Behavioral Risk Factor Surveillance System (BRFSS). (2013) Centers for Disease Control & Prevention. National Center for Chronic Disease Prevention and Health Promotion.Pubmed || Crossref || Others
- 18. Ogden, C.L., Carroll, M., Kit, B.K., et al. Prevalence of obesity among adults: United States, 2011-2012. (2013) NCHS data brief (131): 1-8.Pubmed || Crossref || Others